The three levels of care provided by hospitals: conventional, contingency, and crisis, were outlined in a letter sent to all hospitals. They must notify the state by Wednesday that they have adopted some version of crisis standards to ration care.

Most hospitals in California are overwhelmed by COVID-19 patients. The situation is worst in Southern California and the San Joaquin Valley, where the intensive care unit (ICU) availability is listed at 0.0% on the state Department of Public Health's Regional Stay Home Order map and also on the department's announcement on Sunday of the latest COVID-19 facts.
"Most hospitals in California are no longer able to offer regular hospital services, switching instead to 'contingency care,' said Dr. Mark Ghaly, the California health and human services secretary," report Rong-Gong Lin II and Melissa Gomez for the Los Angeles Times on Dec. 30. Under contingency care, hospital staff "work longer hours and wards are reconfigured to take more patients. The next step could be 'crisis care,' in which more medical rationing would occur."
The state Department of Public Health [CDPH] on Monday [Dec. 28, 2020] issued a memo about its “California Crisis Care Continuum Guidelines,” which, they said, must follow ethical principles, health equity goals and civil rights laws. Facilities that need to begin to ration critical care resources must notify local and state public health departments immediately.
According to the memo signed by Deputy Director Heidi W. Steinecker, "CDPH expects that all facilities have crisis care continuum guidelines and if experiencing surge (as [sic] majority of facilities currently are), are implementing those guidelines..."
By January 6, 2021, all facilities must notify their local CDPH district office and local public health department via email that they have adopted and publicly posted (include link to posting) one of the following: their own crisis care continuum guidelines, another facility's guidelines, or the State's California Crisis Care Continuum Guidelines [pdf].
Soumya Karlamangla, Luke Money, and Lin report in graphic terms on Dec. 31 on the deteriorating conditions in several Los Angeles County hospitals, reminiscent of what was seen in New York City hospitals last spring.
Dr. Christina Ghaly, the L.A. County health services director [and the wife of Dr. Mark Ghaly], said Wednesday, “There have been some unfortunate outcomes from patients in hospitals and ambulances across the county who couldn’t be offloaded into an emergency department in a timely manner.”
As reported by the Times on New Year's Day:
"Sometimes as many as 10 ambulances are queued up waiting to drop off patients, and “we’ve had patients waiting in ambulance bays outside of [emergency departments] for seven hours, eight hours,” said Cathy Chidester, director of the L.A. County Emergency Medical Services Agency.
Supply and demand
One of the most critical resources that will be considered in triage plans is the allocation of "highly trained staff — such as respiratory therapists, ICU nurses and critical care doctors — in a way to keep as many people alive as possible," add Lin II and Gomez in the source article. "That means that those less likely to survive might not receive the same level of care they would have otherwise."
Another resource in short supply, particularly in older county hospitals with aging infrastructure, is oxygen – a basic need in a pandemic caused by a respiratory virus. On Saturday, the Army Corps of Engineers personnel arrived to update oxygen delivery systems in six hospitals.
Other hard-hit regions and states
As bad as things are for California hospitals, they are not alone. According to the hospitalization metrics shown on The Washington Post coronavirus tracker on Jan. 3, the state is fourth in "currently hospitalized for Covid per 100,000 people," behind Arizona, Nevada, and Alabama, respectively, and fourth in "currently occupied ICU beds" per capita behind Arizona, Nevada, and Arkansas, respectively.
Case incidence
The Los Angeles metropolitan area is #4 in "Where the Outbreak Is Worst Now" on The New York Times metro/micro area tracker on Jan. 3, at 132.2 coronavirus cases per 100,000 people. California's Inland Empire, also in Southern California, is #1 at 141.8 cases per 100k. As high as that may be, it's been higher in other metropolitan regions.
The first large-population metropolitan area to see a devastating outbreak during the fall resurgence was El Paso, Texas. In our second post on that region's outbreak, daily new cases averaged over 200 per 100k on Nov. 12, 2020.
The good news is that case incidence, and the hospitalizations and deaths that follow, drop off, presumably due to the coronavirus restrictions imposed by local and state governments. Daily new cases in El Paso County are averaging 38.7 per 100k on Jan. 3, according to Covid Act Now. Among the state's 254 counties, it is #163, in the lowest one-third. By contrast, Harris County, the state's most populous county, which includes Houston, is #102 with 53.4 daily new cases per 100k.
El Paso remains on The New York Times metropolitan tracker in the fourth category, "The Places Hit Hardest," which is a ranking of cumulative coronavirus cases, i.e., from the beginning of the pandemic, rather than the last two weeks. It is #11, at 118.2 cases per 100k. The only California region to make that top twenty list is El Centro in Imperial County: #7 at 125.3 per 100k.
Related in Planetizen:
- California's Hospital Crisis: What Lies Ahead, December 21, 2020
-
El Paso Update: 'On the Brink of Disaster', November 13, 2020
- Another Grim Coronavirus Milestone: This Time in Southern California, August 19, 2020
FULL STORY: Paramedics having some patients stay home as hospitals struggle with COVID-19 wave
Planetizen Federal Action Tracker
A weekly monitor of how Trump’s orders and actions are impacting planners and planning in America.
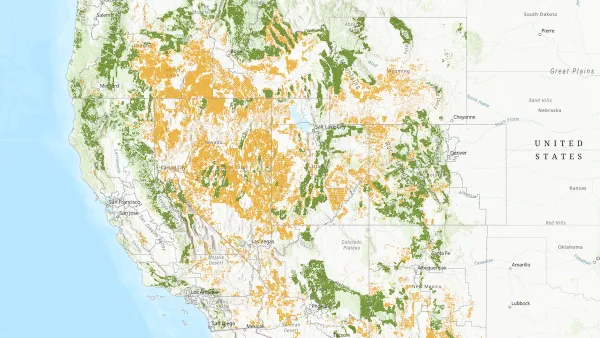
Map: Where Senate Republicans Want to Sell Your Public Lands
For public land advocates, the Senate Republicans’ proposal to sell millions of acres of public land in the West is “the biggest fight of their careers.”

Restaurant Patios Were a Pandemic Win — Why Were They so Hard to Keep?
Social distancing requirements and changes in travel patterns prompted cities to pilot new uses for street and sidewalk space. Then it got complicated.

California Homeless Arrests, Citations Spike After Ruling
An investigation reveals that anti-homeless actions increased up to 500% after Grants Pass v. Johnson — even in cities claiming no policy change.

Albuquerque Route 66 Motels Become Affordable Housing
A $4 million city fund is incentivizing developers to breathe new life into derelict midcentury motels.

DC Area County Eliminates Bus Fares
Montgomery County joins a growing trend of making transit free.
Urban Design for Planners 1: Software Tools
This six-course series explores essential urban design concepts using open source software and equips planners with the tools they need to participate fully in the urban design process.
Planning for Universal Design
Learn the tools for implementing Universal Design in planning regulations.
Heyer Gruel & Associates PA
JM Goldson LLC
Custer County Colorado
City of Camden Redevelopment Agency
City of Astoria
Transportation Research & Education Center (TREC) at Portland State University
Camden Redevelopment Agency
City of Claremont
Municipality of Princeton (NJ)